The 2 most dangerous things in the world are too much skepticism & not enough of it
Antidepressants tell both sides of the story
Trigger warning: This post is about suicidal thoughts.
Zoloft nearly killed my 17 year old patient.
A few months back, while on shift, I got a call from an acquaintance asking if I was working. Her voice was shaking and I could hear chaos, raised voices and someone crying hysterically in the background as she explained that she was on her way to my ER. An hour before, she’d walked into her daughter’s room and found her standing in the closet, holding a chef’s knife in one hand, her phone in the other, crying and repeating over and over that she didn’t want to die.
As I write this it still sends chills through my body, and then again as I remember how not uncommon the story truly is.
The kid is an honor-roll student, varsity soccer player and member of the robotics club beginning her senior year at a ‘well-to-do’ school in the burbs. This past summer, after struggling with anxiety and stomach problems ‘forever’ or, you know, since middle school and reportedly just tired of just ‘waiting to feel better,’ she’d started researching and talking to friends about treatments to lessen her anxiety.
After multiple conversations with her parents and pediatrician, she had decided that all of her issues were tied to chronic anxiety and the doc had agreed to start her on an antidepressant medication in an attempt to settle her mind prior to the start of a new school year.
Zoloft, a first-line drug of choice, is similar to other psychiatric drugs in that it is often prescribed at a low ‘entry level’ dose for a period of time that allows the body to acclimate, before increasing to the ‘therapeutic’ dose - the lowest dose that you should expect to actually help with symptoms. From there these drugs are titrated up until the patient’s symptoms are well-managed or until there’s some side-effect or you’ve reached max dose that prevents the clinician from going higher. At this point the med might be changed or another may be added.
For my patient, things had started off well enough. On the ‘entry level’ dose, she was still anxious, but didn’t notice any issues and so after the intro period, she doubled the dose as she’d been directed. Within days of the increase, she began experiencing relief from her long-standing anxiety and was grateful to have finally gotten some peace.
What she hadn’t expected was that over the next month another change would occur.
She started having crying spells, emotional outbursts and eventually depression with intrusive, obsessive suicidal thoughts. Things deteriorated progressively until that night when she found herself screaming for help from the closet.
There’s no medical excitement here, no clinical mystery, no big Dr. House moment to relive.
I didn’t have to dig deep to diagnose this one and it’s not a story that highlights how clever I am or how advanced my diagnostic skills are.
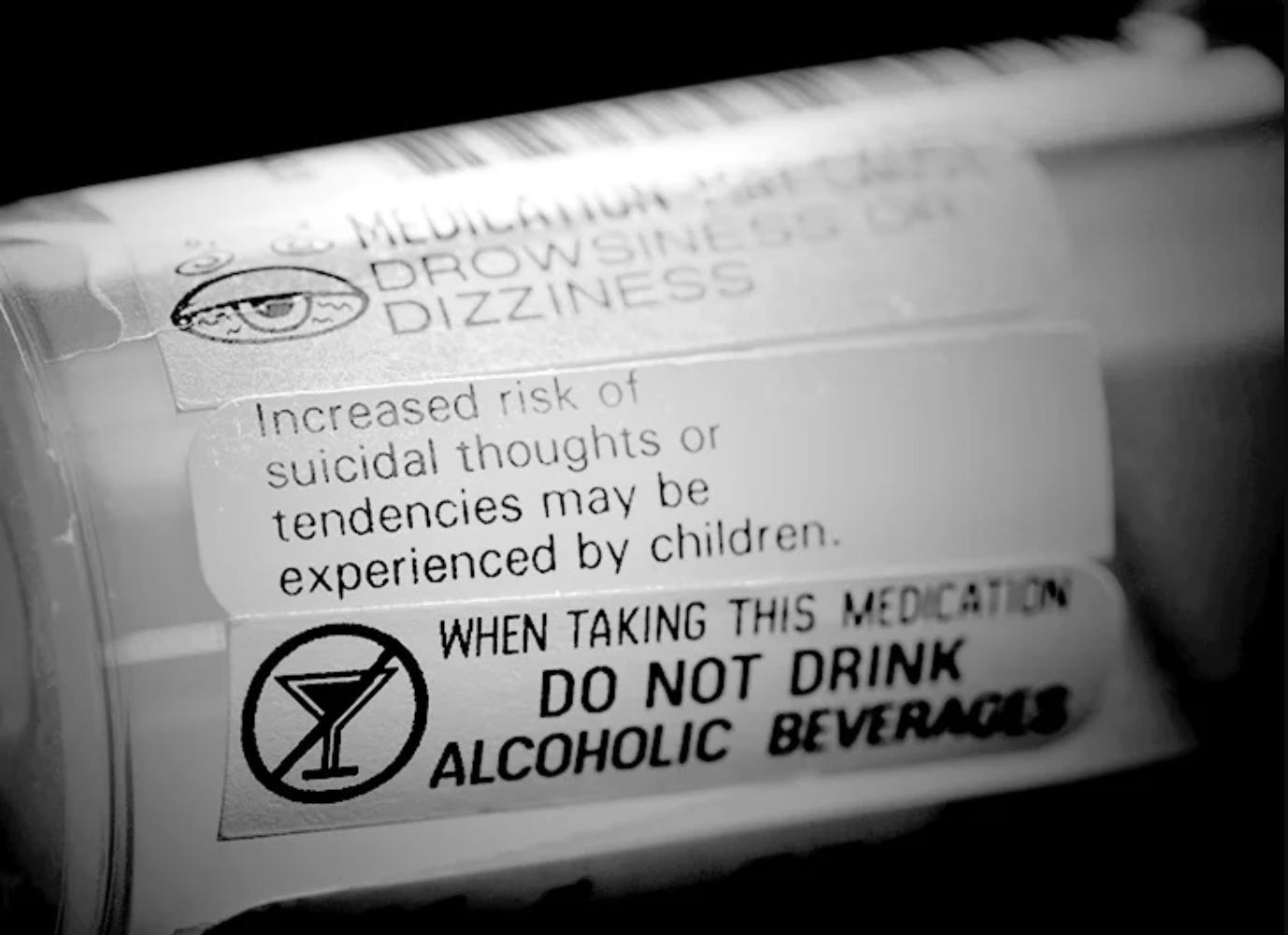
In fact, horrible, life-threatening suicidal ideation is a known risk when giving this class of drugs to teens, and the FDA, who in my opinion and that of other industry leaders, is notoriously bad at regulating the pharmaceutical industry, has rightfully placed black box warning on this class of drugs (although even that declaration is controversial). The ‘box warnings’ are the most serious that exist in our regulatory structure and are done when the risks of an adverse event are particularly serious or grave.
The intention of the black box warning is to allow the substance to remain on the market and still be prescribed, but only…
when benefits outweigh the very scary risks (shouldn’t that always be the case?)
with fully transparent informed consent (humm… shouldn’t that always be the case)
when everyone (clinician, patient, family) is committed to actively look out for signs/symptoms of the development of the scary concern in question (which again, shouldn’t that always be the case?…)
Back to my patient.
The most likely explanation of her symptoms was that it was related to her recent dose increase of the SSRI and next steps were pretty clear - she needed admission to a psychiatric facility where she could be watched, slowly weaned off the drug until stable, and then she should be discharged and followed closely outpatient.
I know I’ve said this case is boring like 16x now, but regardless of how mundane the Medicine piece is, I think about this case a lot. Probably daily.
My mind sort-of obsesses on the details.
As the mother sobbed in my arms outside of her daughter’s exam room all I could think of that night was,
Who screwed this up?
Who hurt this kid?
I hate them.
Was it the FDA? Big Pharma? Idiot parents? A lazy pediatrician?
No matter how hard I tried, I couldn’t find anyone to blame. And months later, still nothing - I’m not convinced that anyone did anything wrong.
Objectively, this outcome was statistically predictable: For every xyz thousand young people given these drugs, we expect abc number of them to become suicidal or die from suicide.
It’s that simple.
Which begs the question…
Are we prescribing medications appropriately?
To individual patients? IDK - maybe, maybe not.
As an industry? Meh - studies support that many (if not most) drugs are being overprescribed.
Does that include inappropriate prescribing of SSRIs? Of course it does..
But here’s the flip side.
For every SSRI story like the one above, there are 1 (or 1000) from others who report that SSRIs saved them from death by suicide by “turning down the volume” on depressive, anxious, enraged, obsessive or other horrifically traumatizing intrusive thoughts.
So who’s to say they shouldn’t be prescribed?
The fact is:
1 out of every 4 Americans takes prescription meds for their mental health, and that percentage has skyrocketed in recent years.
But whose job is it to do the ‘risk verses benefit’ math?
While we deserve access to accurate data from Pharma, the FDA and clinicians of course, at the end of the day, the person with the responsibility is the one who has the most to gain and the most to lose - it’s the patient.
Because no matter how you slice it:
Medicine is an art & a science - with right & wrong being more ‘gray’ that we’d like to admit.
Consider these examples:
Chemotherapy is poison if you’re healthy, but can be life-saving if you have cancer.
‘Blood-doping’ is immoral in athletics, but an effective treatment for severe forms of anemia.
‘Dangerous’ medications are considered malpractice some instances, but in others, they’re a miracle drug.
The question is not, ‘Are SSRIs good or bad?’ It’s more nuanced than that.
The question is and should always be,
‘Do the potential risks of this medication outweigh the potential benefits?’
Asked in the context of severity, and compared to other medications or non-medication treatments (diet/lifestyle/therapy…etc) known to provide benefit.
And not just that, but as a society we should also be considering:
Is it a mistake to alter the minds of a quarter of our population?
Is it necessary? And if it is, why?
In other words,
Are we helping people more than we are harming them?
Are we giving these meds to the right people who will likely benefit?
Are we using pharmaceuticals as a ‘bandaid’ to mask the results of a dysfunctional lifestyle, toxic environment or moral decay? And if so, how can we fix the underlying issues?
To be honest, I don’t know the answers to any of these questions, but I do know that while these questions should absolutely be examined from a societal perspective, they are also questions that you should consider as an individual considering treatment, a parent considering treatment for a child, an employer considering what mental health solutions to offer to your employees and as a clinician who is in the difficult, sometimes impossible position of educating patients on how to make an informed decisions where the wrong choice can be fatal.
The most common risks of SSRIs are known.
Things like:
Nausea
Headaches
Weight gain
Sleep problems
Sexual dysfunction
The scarier risks are known too.
Mania
Diabetes
Suicidal thoughts
And in specific populations (young adults, women, those with underlying psychiatric disease…etc) there may be a higher or lower number of people likely to experience particular adverse effects.
And it’s your job as the decision maker to do your best to understand the risks & look out for them while also paying attention to your symptoms making sure that you are actually getting the benefits you’re hoping to get.
Your judgement won’t be perfect - because no one’s is, including your doctors.
My advice is to ask questions and learn as much as you can.
“Start where you are. Use what you have. Do what you can.”
My conclusion? SSRI’s are the same as any other drug.
There are risks and potential benefits. Their use should be something that is carefully considered with a healthy level skepticism.
Until next week.
Tiffany
PS. This is my first foray into mental health topics and to be honest there is so much to say. I’m excited to hear what you think over the coming months. I read all comments and all emails, so please fee free to send me a note. SSRAnd if you know someone else who would find this discussion interesting, please take the time to share it.
**Don’t forget: always medically themed, but never medical advice.





Hi Tiffany - would love to get the correct link under 'skyrocketed' about the increase in prescribing of SSRIs (link not working for me?) . Is it a societal ills causing the rise or just better availability/cheapness of the drug?
I'm a primary care doc and prescribe SSRIs to many, many people. I see my job as doing the best I can for the person in front of me with what I have. I frequently feel that the person would be benefitted by quitting their job or going to couple's therapy, for example, more than by an SSRI. I might gently point in this direction, but if the person ignores my finger and requests a pill, I go with it.