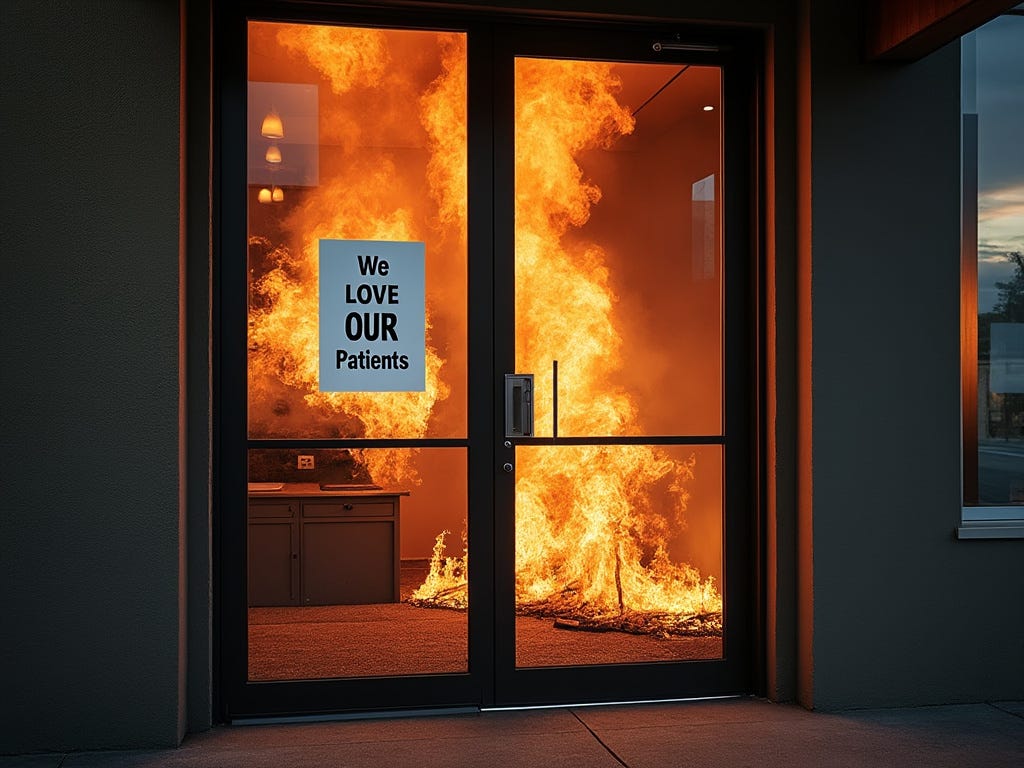
In our healthcare system, patients don’t matter.
There’s an illusion that they do.
The sign on the door says, “We *heart* our patients,” but if you show up an hour late because your kid was vomiting on the way to the appointment, will you still be seen?
Probably not.
Most likely you’ll be chastised and refused service even though YOU routinely wait hours for care at that same office.
Our whole system is designed to support a power dynamic where the big, smart doctor is the dominant authority who does… well, whatever they want. And you, the patient, are the uninformed, subservient party whose role is simply - to obey.
After all…
The medical degree on the wall is proof that ‘The doctor knows best’
Your concerns are obviously not that important given how often you leave messages and don’t receive a response.
And clearly you’re not worthy of respect which is why you have to agree to pay literally ANY amount for service in writing before a clinician will even agree to see you. Refuse and you won’t be seen or treated.
The ‘healthcare’ system proudly demands that its customers submit to unethical business practices and abuse, or die - and we get away with it.
And while in many cases this dysfunction isn’t an ego-driven demand instituted by the doctor themselves but is a reactionary adaptation by clinicians just trying to survive in the current system, the effect on patients is still demoralizing.
So, it’s really no wonder that patients don’t feel empowered with any degree of choice when they walk in the door.
And although I get that you don’t feel like THE decision-maker as the patient, if you give me 2 minutes, I’ll show you definitively that you are.
Let me prove it to you.
Are you the ultimate decision maker?
Well,
When the all powerful doctor says you need to get a test done, take a medication, or go to PT does that mean you absolutely have to do it?
My answer is, ”of course not”
In fact, I KNOW the answer is, “of course not” because I know you’ve received recommendations from your clinician that you choose not to act on all the time.
Have you ever been told to ‘work out,’ ‘drink less booze’ or ‘eat better’?
And do you always comply?
The answer, ‘of course not’ and when it’s put in context, is sort of obvious.
And I point this fact out because it leads us to ask a fundamental and frankly much more important question, and that is…
Just because your doctor recommends something, does that mean you absolutely need it?
And, in my experience, both as a patient and as a clinician in the emergency department, I can emphatically say:
No. It does not.
Is it a good idea? Maybe.
BUT also, sometimes, if you need it a refusal might cost you your life.
So clearly this is not a comforting answer, so, how the heck as a patient, do YOU know what to do?
Asking (more) questions is the only way to decide.
Your doctor is an expert.
But ‘expertise’ and ‘competence’ are never absolute.
The point here isn’t that doctors are idiots, my point is that doctors and clinicians have multiple, often conflicting incentives when putting together a treatment plan for you - and as sad as it may be, your wellbeing is only one of those guiding factors.
Let me illustrate this with a very real, very true ER story.
It doesn’t matter if it’s expensive, harmful and unnecessary - you’re gettin’ it anyway.
When I first started practicing, I was working overnights at a rural ER. One night while I was still orienting I saw a teenage girl, we’ll call her Charleigh. She’d come in because she’d “missed school” and was having some “belly pain” - literally, that’s what the ‘patient complaint’ section of the EMR said.
So I walk in the room to see her, and Charleigh and her mom tell me that after waiting for several hours in the ER waiting room, she was actually already feeling ‘a lot better’ and at this point, she just ‘needed a note’ and some sleep.
I told them, I’d recommend talking through her medical history and doing an exam especially since they’d already waited forever to be seen… and they graciously agreed.
Her history and exam were thankfully pretty boring. I didn’t see any red flags.
The triage nurse had recorded vitals several times over her hours long wait - no fever, nothing unexpected, everything within the normal range. The nurse had also followed the hospital policy of grabbing ‘routine labs and urine’ on arrival so that we could ‘expedite care’. All of those were normal too. She wasn’t pregnant, no signs of infection, no recent trauma - everything looked great.
Check, check, check.
During orientation any case designated as an ESI 3, Emergency Severity Index 3 or above had to be run by an experienced ER Doc prior to discharge. Unfortunately for this patient, ‘abdominal pain’ was always an ESI 3.
So, I prepared the discharge paperwork and found an ER Doc to present the case to - fully expecting them to half-listen while rolling their eyes and charting before shooing me away, but instead here’s what happened …
“So hey Doc, I’ve got this 16 yo female who presented 6 hours ago with a complaint of…. blah, blah, blah….”
ER Doc looks up and says, “Ok, what did the CT show?”
Confused Me says… “Huh?… ummm… I uh… I didn’t do a CT. Labs, urine and vitals were normal, she’s not pregnant, there’s no abdominal tenderness to palpation & I did all 3 of the special tests for appendicitis - everything’s negative and she’s actually feeling much better now…”
The she says… “Yeah, I hear you, but you still need to get a CT.”
At this point I’m really confused.
“I’m sorry. I’m not sure I understand. Based on this exam and history, a CT isn’t indicated and it carries more risk than benefit. Am I completely missing something?”
She answers, “Look, we don’t discharge abdominal pain from the ER without a CT. Think about it. You aren’t going to get sued or lose your license for doing an ‘unnecessary scan’ that’s ‘negative’ and maybe it costs the insurance company a few thousand dollars or causes cancer 30 years from now, but those aren’t going to lead to problems, but you know what you will get sued and what will cost you your license?”
I’m still starting at her shaking my head reflexively shaking my head sort of in shock.
She continued… “What WILL bite you in the ass is the one in a million appendicitis that doesn’t follow the textbook and reveals itself 6 hours from now and ends with a terrible infection that kills the patient. You’re gonna be held responsible and when you get home from court the only question you are going to remember being asked is, ‘why didn’t you order the CT scan?’ So we could just skip all of that that and go get the scan and when the negative results come in, let her go home.”
And that’s when I really got it for the first time,
She wasn’t evil.
She wasn’t even strictly wrong.
She was just teaching me what she felt to be an appropriate strategy to manage my risks so I could survive to practice another day and help more patients.
But, it was also the moment I knew, healthcare had a serious problem.
This doctor and this approach were not unique and the consequences of using this ‘tactic’ for risk mitigation at scale would be devastating - and it is - to the tune of at least millions of dollars wasted per year by families, companies of all sizes and taxpayers - not to mention any clinical harms.
BUT I thought, maybe in this case, I could help…
So I go back into the room to talk to Charleigh and her mom who have already packed up their things and are ready to go.
I tell them that the doctor I’m working with has suggested we get a CT scan ‘out of an abundance of caution.’
I explain the associated risks (costs/time/radiation) & benefits (confirmation of nothing serious at least at the moment of the scan).
I reiterate that a CT is NOT considered necessary based on the patient’s presentation and current standard practice guidelines.
And then, I give them the option to complete the CT scan or to simply decline.
And the Mom asks": “The ER doc wants us to get it?”
Me: “Yes. she does”
Mom continues: “Will the insurance even pay for the visit if we decline or have to sign out AMA?”
Me: “I don’t know “(because none of us do and I’ve asked… a lot)
Mom: “Well if she thinks it’s important enough to recommend then…we’ll get it”
They quickly decide they want it and that’s that.
And I ask myself ‘Why?’ Because the doctor (who has NEVER laid eyes or hands on the patient) is suggesting it, and so it’s probably faster/better/cheaper to go ahead and do it and she can’t imagine any reason that a doctor would recommend a treatment other than it’s best for Charleigh.
Sometimes ‘recommendations’ are really just options.
I’m not anti-imaging for belly pain, just like I’m not anti-vaccine or anti-anything else, but the benefits of doing something must outweigh the risks of doing it, or it shouldn’t be done.
We are asked to make choices all of the time and it’s our job to do the best we can to make informed ones. We ride in cars for example, even though there’s definitely a risk of dying in an accident because it costs too much to never leave our home.
The mistake that we make in healthcare as patients is, we assume our clinicians have already done all of this math for us, and we assume that our wellbeing is the most important consideration, but I’m telling you it’s not that simple.
Questions are how you tell the difference.
If you want to understand if the doctor is erroneously recommending a test or treatment to cover their butt in a 1 in a million bad outcome?
I’d argue, you just ask. Solicit more information.
Here’s how:
“So doc, I’m trying to do the right thing here. I’ve taken a lot of antibiotics in the last few years… What are the risks if I don’t start this antibiotic today? Is there harm in seeing if it gets worse and start then?”
“If I don’t get the CT now, how would I know that things are getting worse and I should come back in to get checked out?”
“If I delay doing this now, will it be too late by the time I figure it out? Is it likely that I’ll die or something terrible will happen?”
“How strongly do you feel I need this test? Will the results of this test change your treatment plan?” (hint if they wont - maybe pass on the test!)
“Can you tell me a little more about what you are looking for with this test? Are there long-term risks associated with it”
Have you questioned your clinicians authority? How did they react? What are you favorite questions to ask? What do you find useful? I’d love to know in the comments below.
If you found this article thought provoking or helpful, I’d love for you to consider sharing it with a friend.
Until next week,
Tiffany (don’t forget - never medical advice)





Great information, Tiffany! Thanks for sharing this!
Excellent Article! I relate to everything you said, because I have experienced exactly this with my health and similar situations with my hubbys health (he has a rare blood disorder due to a genetic mutation). We have had a couple outstanding Drs (and incredible nurses) and we have had some Drs that nearly cost us my husbands life. We have learned to ask EVERY question, we have learned to not blindly trust that our best interest is at their heart. It is likely not. We have learned to be our own patient advocates. Its a hard learning process! And extremely expensive and frustrating. Thank YOU for seeing that our system is broken.